Call our 24/7 advice line for health care professionals and families if you need support with symptom management and end of life care - 01284 766133.
Resources for Care Homes during the Covid-19 Pandemic
Here are some resources for care home staff which might be helpful during this coronavirus pandemic.
The latest guidance from the British Geriatric society
Managing the COVID-19 pandemic in care homes.
https://www.bgs.org.uk/resources/covid-19-managing-the-covid-19-pandemic-in-care-homes
Spiritual support
St Nicholas Hospice Care Chaplaincy team is here to offer spiritual and emotional support to all those receiving care, their family and friends and to members of staff and volunteers. You can find out more about this support by clicking here. Prayers which may be useful in a care home setting can be found here.
What you can do to practically care for someone who is in their last days and hours of life
• https://helixcentre.com/_content-img/projects/eolc-toolkit/Practical-Care-For-Dying-Person-Toolkit.pdf
• Comfort measures for residents at end of life
What is death like?
A very useful eight-minute video. Dr Kathryn Mannix, palliative care consultant and author of ‘With the End in Mind’, talks to journalist Nicola Meyrick about death and what death is like. One of the things that people will notice is that you are more tired than you used to be.
Delivering news of a death
http://www.sad.scot.nhs.uk/media/16240/delivering-news-of-a-death-by-telephone.pdf
Advance Care Planning / My Care Wishes
A three-minute guide to having a conversation about advance care planning / future care wishes.
https://www.youtube.com/watch?v=MERUHyT3yFk
Advanced Care Planning is about what would matter to the resident if they became seriously unwell with coronavirus, for example, asking “Are you the kind of person who would want to go to hospital, to intensive care or would you want to stay at home?”. Some of the people who have already died from the virus have not been in intensive care, as this would not have made any difference to their outcome as they were coming to the natural end of their life. This includes an urgent situation, for example, hospitalisation versus remaining in their usual place of residence and receiving symptom control/palliative care.

The My Care Wishes Folder (yellow folder) includes DNACPR (https://www.westsuffolkccg.nhs.uk/wp-content/uploads/2020/02/Merged-for-printing-full-set-Jan-2020.pdf) which should be easily accessible within the resident’s room. This is particularly important in out-of-hours emergency situations, especially if bank and agency staff are on duty. It ensures that all care staff will have all the key information in one place.
Purple Book
The aim of this booklet is to support care homes in their decision-making and, by using local resources, reduce unnecessary and unplanned admissions to acute hospitals.
http://www.westsuffolkccg.nhs.uk/wp-content/uploads/2019/09/Purple-Book-Section-1-Main-v1.0.pdf
Management of Outbreaks of Acute Respiratory Illnesses in Care Homes Out of Season and In Season
https://www.westsuffolkccg.nhs.uk/local-health-services/care-homes-team/management-of-outbreaks-of-acute-respiratory-illnesses-in-care-homes-out-of-season-and-in-season/
Anticipatory prescribing of medications often used in the last few days of life
Anticipatory prescribing is when a GP, specialist doctor or specialist nurse prescribes injectable medicines that might be required if the patient deteriorates and can no longer swallow medications. These medicines can be supplied and kept at the person’s home or in their nursing or care home in case they are needed. They are often called ‘Just in Case’ medicines or end of life medicines.
The medicines can be used to treat the symptoms that are common in the last days of life, including:
• pain
• nausea and vomiting
• noisy chest secretions
• agitation
• breathlessness
You should know where they are kept and what to do if they are required. If you are the healthcare professional responsible for administering them, make sure you know how they should be given in advance. If it is not within your role to give medicines, know who to call if you think the patient might need these medicines to manage their symptoms.
Suffolk End of Life Care Guidelines
Offers guidance on an holistic approach to end of life care with the five key principles of CRISP: Communication, Recognise, Involve, Support, Plan and Do, with a support tool.
http://www.westsuffolkccg.nhs.uk/wp-content/uploads/2017/11/Suffolk-End-of-Life-Care-Guidelines-2017.pdf
A resource for ‘just in case medications’ which is adopted for use in Suffolk
http://www.suffolkcommunityhealthcare.com/Portals/2/Documents/1715%20JIC%20Meds%20Policy%20FINAL.pdf
NHS Education for Scotland
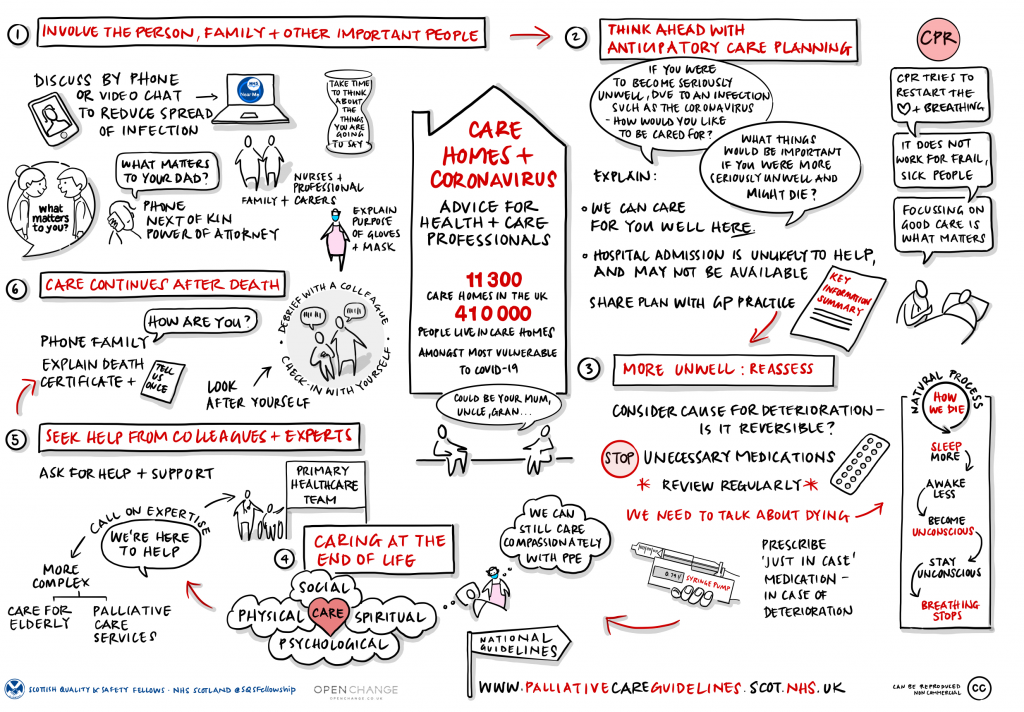
A helpful visual to assist with information on Care Homes and Coronavirus. Created by members from cohort 12 of the Scottish Quality Safety Fellowship, with Hazel White from Open Change.
https://learn.nes.nhs.scot/28412/quality-improvement-zone/learning-programmes/scottish-quality-and-safety-sqs-fellowship-programme/care-homes-and-covid-19-poster
